Complications And Risks of Placenta Previa During Pregnancy
Placenta Previa: Complications And Risks All You Need To Know
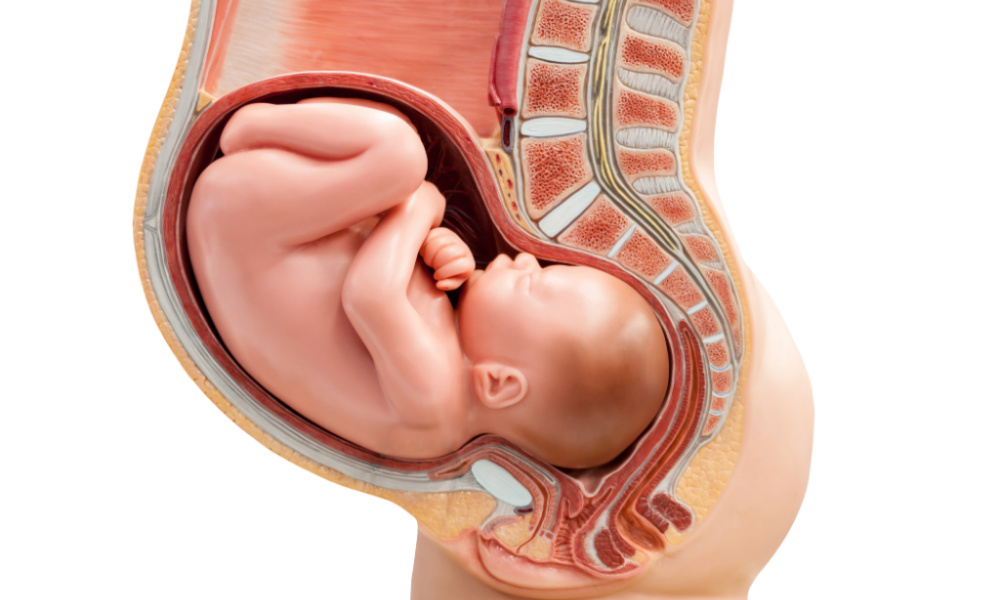
What is a placenta?
A placenta is a temporary organ in the uterus that develops during the 20th week of gestation and continues to grow throughout the pregnancy. It attaches the growing fetus to the mother via a rope-like structure called the umbilical cord to provide all the nutrients and oxygen from the mother to the baby and transfers the waste from the baby to the mother which is excreted out from her blood circulation. It also produces the hormone called progesterone, which helps in the maintaining the pregnancy till term.
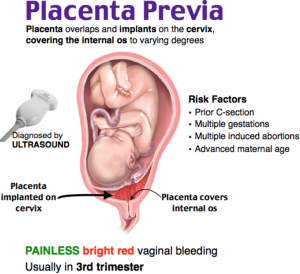
What is placenta Previa?
Bleeding in placenta previa
What are the complications And Risks of Placenta Previa?
What are the causes And Risks of Placenta Previa?
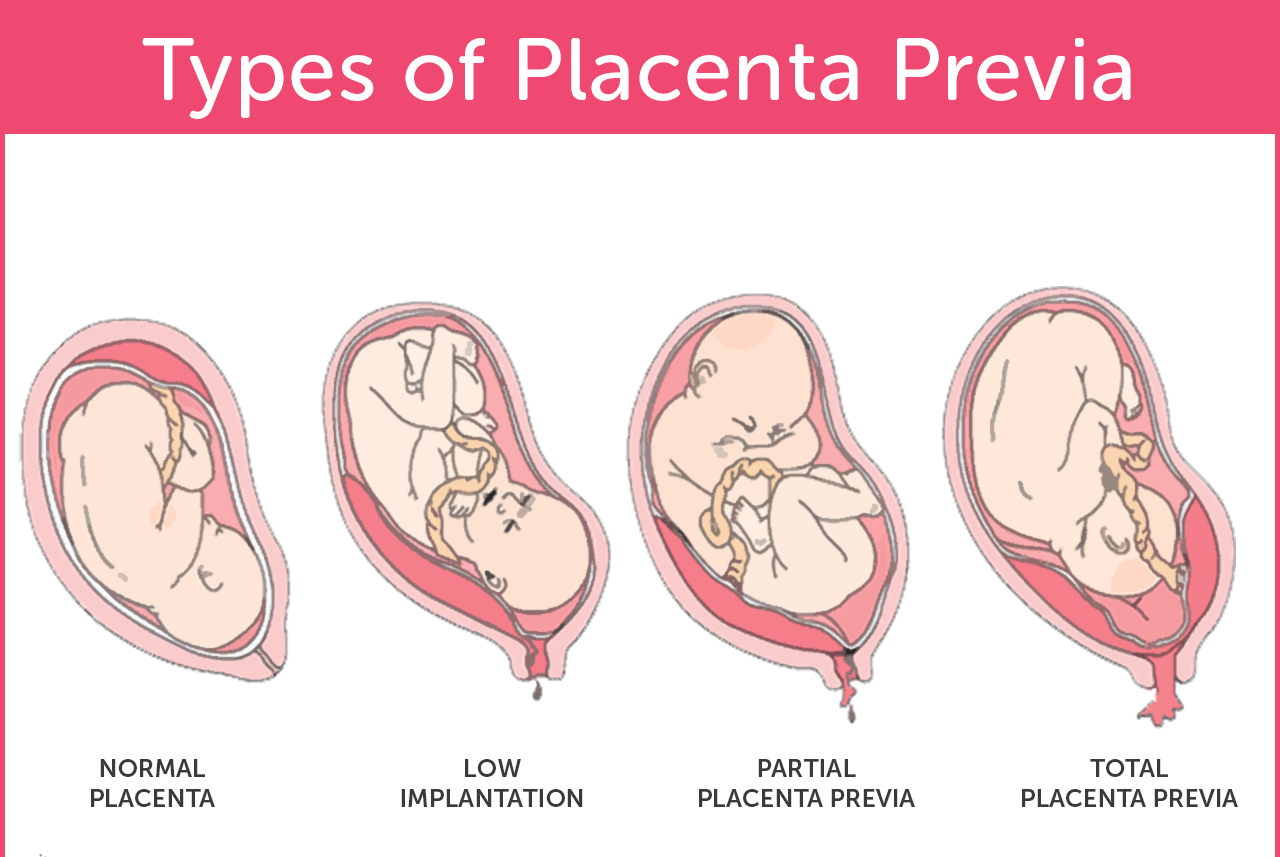
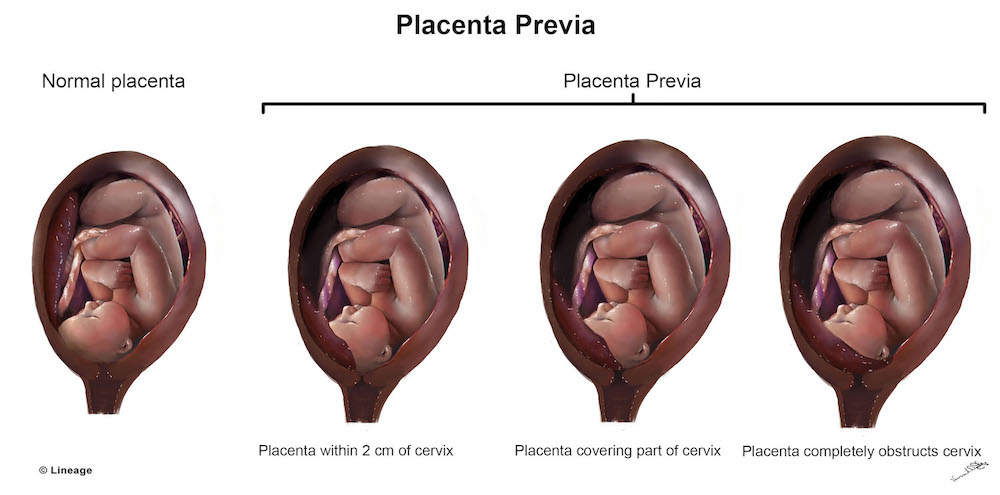
What Are The Types Of Placenta Previa?
What Are The Symptoms Of Placenta Previa?
What Is The Treatment For Placenta Previa?
How to prevent placenta Previa?
Dangerous Placenta Previa
Placenta Previa at 20th week:
A woman who may have placenta previa presents with painless vaginal bleeding as early in the 12th week of gestation as this is the time the placenta is completely produced. But instead of attaching to its typical site in the uterus which is the fundus of the uterus, the placenta attaches to another site, that can be the lower part or sides of the uterus.
Placenta previa is detected in at least one pregnant woman out of every four pregnant women before the 20th week of gestation. But not all women with placenta previa by 20th week continue to have a placenta in the wrong position till the last trimester. Even if the placenta attaches to the wrong site, it migrates to its normal position as the time passes. When this happens, it is no more a placenta previa.
But at least one woman out of 200 pregnant women continues to have a placenta that remains attached in the abnormal site till the third trimester. If this occurs, then labor in such pregnant women becomes very dangerous and can also be fatal.
It is especially true if the placenta completely covers the internal os, which is the natural passage for the baby to come out from, this condition is regarded as complete placenta previa. If it bleeds, then there may be massive blood loss, and if there are large vessels crossing over the placenta, then the blood loss will be much greater and can send the mother into hypovolemic shock rapidly.
Placenta Previa Ultrasound:
To check for placenta previa on ultrasound, it is a must that the placenta has completely developed so it can be seen on the imaging. For this reason, a radiological diagnostic test should be performed after 20 weeks of gestation.
Placenta previa is usually detected on an ultrasound or magnetic resonance imaging (MRI). Placenta previa is usually detected on routine radiological tests. On an ultrasound, the doctor calculates the distance between the edge of the placenta and the internal os. If the distance is significant enough, then the placenta must be in its correct position, and it will not be placenta previa.
But if the distance between the lower edge of the placenta and the internal os is reduced to a dangerous point, then it is suspected as placenta previa. Still, in such cases, an ultrasound should be repeated at 32 weeks of gestation to know if the placenta is still in the abnormal position or it has migrated to its normal position.
To perform an ultrasound, it is advisable to go for a transvaginal ultrasound, which will produce more accurate results than the transabdominal ultrasound. It is because transabdominal ultrasound may sometime incorrectly diagnose placenta previa.
On the other hand, placenta previa is also detected in an MRI. It is the gold standard imaging to look for placenta previa, but in most cases, an MRI is not needed, and ultrasound is enough to make a diagnosis of placenta previa. On the MRI, the distance between the internal os and the lower edge of the placenta is better appreciated.
Placenta Previa And Birth Defects:
Studies have shown that placenta previa is associated with an increased risk of congenital birth defects in single births, and the risk is increased by 1.6 folds.
Other than this, in high-risk placenta previa patients, the most appropriate mode of delivery in such is c section. And because c section is performed before the term ends, for instance, at 33 to 34 weeks of gestations, there are high chances that the baby is born with complications related to premature delivery.
Such complications may include underdeveloped lungs of the fetus, which may result in breathing problems. The fetus may even turn hypoxic due to a lack of oxygen. Similarly, the newborn may have low birth weight, cerebral palsy as a result of birth injury, and hypoxic-ischemic encephalopathy (HIE).
Placenta Previa Management:
The management of a patient with placenta previa requires prompt handling as the patient’s health is rapidly deteriorating. The nurses are required to assess the overall condition of the patient.
- The first thing is to check the patient’s vital and other baselines. It is crucial to keep the patient under constant surveillance and check her blood pressure as often as every 5 to 10 minutes.
- At the same time, it is necessary to check the fetus’ condition, as well. The nurse should monitor the heartbeat of the fetus as well as the movements of the unborn to make sure that the well being of the unborn baby is intact.
- The next important thing is to monitor the contractions of the uterus of the mother to check if she in labor. The constant monitoring will help in predicting when the labor will be induced.
- The nurses will assess the general examination of the patient to see if her health is progressing or deteriorating. It is imperative to examine the patient in the left lying position to take off the pressure of the weight of the uterus from her organs and abdominal artery.
- In case a woman is bleeding, it is vital for the overall health of the patient for the nurses to know how much blood is lost. The amount of blood loss will also help calculate how much fluid should be replaced in the patient. If the blood loss is massive, then the patient may even require a blood transfusion. To know the amount of blood lost, the nurses will have to check how many perineal pads are saturated in every hour.
Differential Diagnosis:
There are other conditions that may be similar to placenta previa in terms of signs or symptoms. It may include:
- A bladder that is full
- Focal myometrial contraction


24 Replies to “Complications And Risks of Placenta Previa During Pregnancy”