Postpartum Hemorrhage Nursing Diagnosis Risk Factors, Care Plan & Management
What Is Postpartum Hemorrhage?
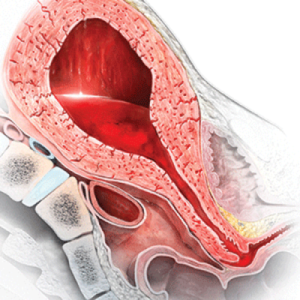
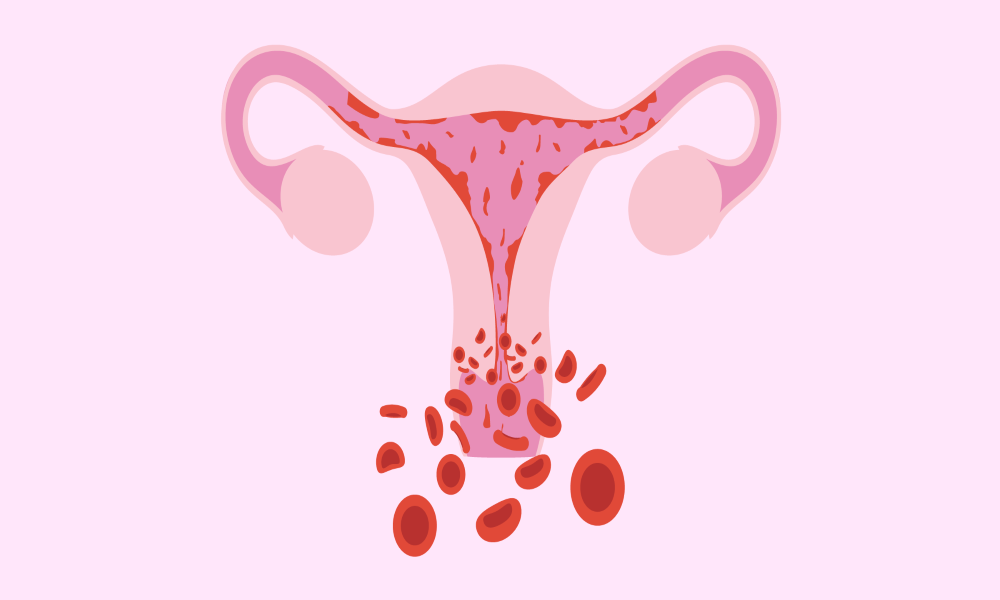
Postpartum hemorrhage is a severe condition where a woman bleeds excessively following immediately after her delivery or a few hours later. Postpartum hemorrhage nursing diagnosis An excessive bleed is defined as a blood loss of more than 500 ml after a vaginal birth. Similarly, a loss of more than 1000 ml after a C section is considered as a hemorrhage.
Every one to five women in a hundred faces this problem. It primarily occurs because of reduced contractions of the uterus. After delivery, the contraction of the uterus is crucial to the seal of the blood that previously supplied the baby.
When contractions fail to occur, the blood that is supposed to be a seal continues to flow, causing a hemorrhage. In medical terminology, it is called ‘uterine atony.’
On the other hand, retained placental fragments result in hemorrhage, as well. Typically, a placenta is delivered a few minutes after the delivery of the baby. For any reason, the placenta is not entirely delivered, and the retained placenta will cause a massive bleed.
Postpartum hemorrhage (PPH) is a significant complication of childbirth, defined as any blood loss greater than 500 mL following delivery. It occurs in about 6-8% of deliveries and can be either primary or secondary PPH. Primary PPH occurs within 24 hours after delivery, usually due to uterine atony, while secondary PPH occurs within 24 hours but within 6 weeks of delivery.
The risk factors for PPH vary depending on the type. Generally, they include advanced maternal age, obesity, multiple gestations, macrosomia (large infants), prolonged labor, and syntocinon (oxytocin) to speed up labor. Management strategies for primary PPH include the administration of uterotonic agents such as misoprostol, oxytocin, ergometrine and prostaglandins. In cases where these medications fail to stop the bleeding, surgery may be necessary. Secondary PPH is managed with uterotonics, blood products and sometimes surgical intervention.
Early recognition and aggressive management of PPH can reduce preventable morbidity and mortality associated with this complication. Healthcare providers need to be aware of PPH’s risk factors, signs and symptoms, and evidence-based management strategies. Early detection and intervention are key to reducing maternal mortality from PPH.
Overall, postpartum hemorrhage is a potentially life-threatening complication of childbirth and one that should be taken seriously and managed appropriately. By understanding the risk factors, signs and symptoms and evidence-based management strategies for PPH, healthcare providers can better care for their patients to reduce the chances of morbidity and mortality associated with this condition.
Postpartum Hemorrhage Nursing Diagnosis is a diagnosis used to identify and treat the cause of excessive bleeding after childbirth. Nurses must assess the patient for signs and symptoms of postpartum hemorrhage, such as heavy bleeding, abdominal pain, or fever.
Once the diagnosis has been made, it is important to determine what caused the bleeding to create a plan of care. Causes could include uterine atony, retained placenta, abnormal placental separation, or trauma to the reproductive tract.
The treatment plan for postpartum hemorrhage will vary based on the cause and severity. Generally, treatments may include medications such as oxytocin to stimulate contractions, manual removal of the placenta, or blood transfusions. Surgery may be needed in more severe cases to control the bleeding.
Nurses must monitor patients closely for changes in vital signs and excessive bleeding. They should also assess for signs of infection, which could become a complication due to postpartum hemorrhage. It is important to provide emotional support to the patient as well, as postpartum hemorrhage can be a traumatic experience.
In addition to treatment and monitoring, nurses should also educate patients about how to reduce their risk for postpartum hemorrhage in the future. This may include proper nutrition before and after childbirth, avoiding excessive labor or delivery interventions, and understanding warning signs of postpartum hemorrhage.
Postpartum Hemorrhage Nursing Diagnosis is an important tool for nurses to treat and prevent excessive bleeding after childbirth. The risks associated with postpartum haemorrhage can be minimised with prompt assessment, treatment, monitoring, and education.
Nurses must follow evidence-based guidelines and protocols when providing care to patients with Postpartum Hemorrhage Nursing Diagnosis. This includes using up-to-date patient education materials and keeping up with the latest research on a postpartum hemorrhage. Nurses should stay current on best practices for diagnosing, monitoring, and treating postpartum hemorrhage. By following evidence-based guidelines, nurses can ensure they provide the highest quality care for their patients.
It is also important for nurses to work with other healthcare professionals to provide comprehensive care for patients with Postpartum Hemorrhage Nursing Diagnosis. This may include working with physicians, midwives, and dieticians to provide the best care for patients. By working together, nurses can ensure that the patient receives appropriate treatment and education about postpartum hemorrhage.
Top 11 Best Full Body Pregnancy Pillow Guide 2020 – Which One To Buy?
What are the risk factors for Postpartum Hemorrhage?
Higher risk for risk for severe postpartum hemorrhage with risk factor(s) identified may include: multiple gestations. Chronic risk for moderate postpartum hemorrhage without risk factor(s) identified may include: blood disorders such as sickle cell disease and hemophilia. Higher risk for risk for severe postpartum hemorrhage with risk factor(s) unidentified may also including hypertension , diabetes mellitus.
An important risk factor related to risk for postpartum hemorrhage is the development of uterine atony leading to risk for hemorrhage after delivery. Risk factors associated with uterine atony may include: epidural anesthesia, multiple pregnancies, excessive bleeding from implantation site.
Many factors contribute to postpartum hemorrhage. Some of them are listed below:
- Cervical or uterine lacerations
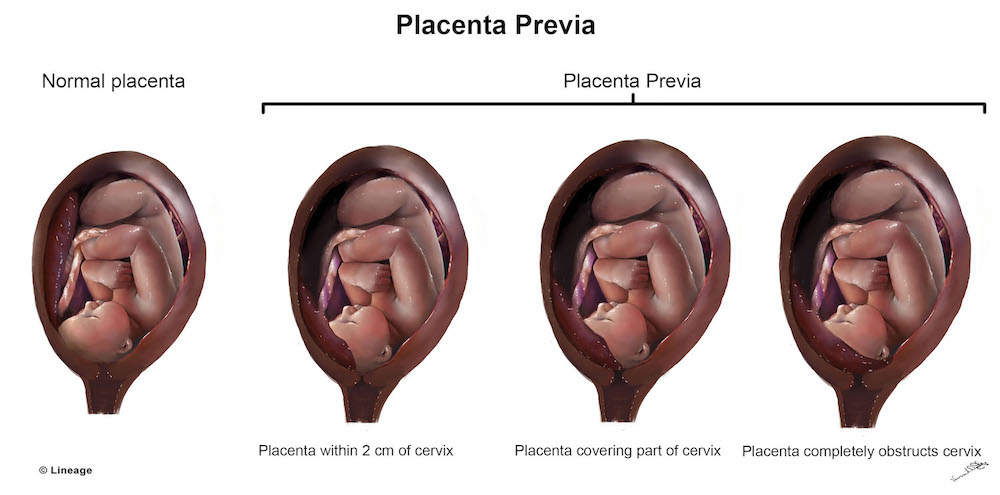
- Abnormal attachment of the placental site such as placenta previa or placental abruption
- Multiple gestations
- Hydramnios, where there is excessive amniotic water collection causing the uterus to stretch extensively.
- Insufficient blood clotting leading to massive hemorrhage
- Risk factors that contribute to risk for increased severity include:
- Placental abruption
- Cervical or uterine laceration
- Infection of uterus
- Past risk factors that contributed to risk for postpartum hemorrhage may include:
- Excessive bleeding from implantation site in pregnancy
- Obesity before pregnancy
- Poor maternal nutrition intake
- Use of epidural anesthesia
- Multi-status births (e.g., twins)
- Insufficient blood clotting which can lead to massive hemorrhage
- Prolonged labor and lack of healthcare provider intervention during the process are risk factors associated with risk for Postpartum Hemorrhage [PPH] risk factor(s). An important risk factor related to risk for PPH is the development
Nursing Plan For Postpartum Hemorrhage:
Nurses play a crucial role in any postpartum problems, and they are the experts to deal with such issues first-hand. Nurses intervene and provide the first-line treatment to any woman with postpartum hemorrhage. It is necessary to ensure complete recovery of the patient and her total gain of strength.
Nurses are required to assess and intervene in such conditions. They necessarily look for signs of shock, monitor the patient’s vital signs, evaluate the amount of blood loss by weighing the blood-soaked perineal pads, and continuously assess the movements and the condition of the uterus.
A nursing diagnosis for postpartum hemorrhage may include the following:
- Risk for imbalanced fluid volume related to excessive blood loss
- Ineffective tissue perfusion related to decreased blood flow
- Risk for infection related to disrupted uterine tissue
The nursing interventions for postpartum hemorrhage may include:
- Monitoring the patient’s vital signs, including heart rate, blood pressure, and oxygen saturation
- Assessing the patient’s bleeding and overall fluid status
- Administering medications as prescribed, such as oxytocin or misoprostol, to help contract the uterus and control bleeding
- Monitoring the patient for signs of infection, such as fever or increased heart rate
- Providing emotional support to the patient and their family.
What does the Nursing Care Plan include?
There are eight essential plans that nurses mainly work on and are included in the postpartum hemorrhage nursing diagnosis.
Assess for decreased fluid volume:
To check for fluid deficiency in the body. The outcome of this assessment must be to replenish the fluid. The nurse would immediately start an IV via a cannula placed in the vessel of the patient. Providing fluids via IV would replenish the lost fluids more rapidly. If the blood loss is massive, the patient may also require a blood transfusion.
Related:Best Postpartum Belly Wrap 2020- 13 MOM Approved Belly Wraps
Assess for fluid overload:
To check for increased fluid retention in the body. It is monitored via input/output charting. The amount of fluid that goes inside the body should coincide with the amount excreted in the urine. If the amount in urine is less than the fluid intake, a nurse would take measures to increase the urine output. Plus, a urine catheter may be inserted for better monitoring of the fluid loss.
Assess oxygen supply:
Monitor the amount of oxygen getting absorbed in the body tissues. It is followed via the level of oxygen saturation. If saturation is reduced, then a nurse may have to aid in intubating the patient.
Assess for infections:
check for an increase in the body temperature that may indicate an infection as acquiring an infection in this state is very common in women. The nurse will monitor the vitals of the patient and administer IV antibiotics as a prophylactic to save the patient from acquiring an infection in this state.
Assess the patient for signs of discomfort or pain:
If the patient feels uneasy or moan in pain, then it is best to administer pain killers via the IV line or administer sedatives to keep the patient calm and free of pain.
Assess the uterine movements:
If the uterus of the patient is not contracting on its own, the nurse will have to massage the uterus and contractions. This is compulsory because the contractions of the uterus will reduce blood loss.
Assess for mental problems:
A woman is agitated, overwhelmed, stressed, and may get depressed after delivery and especially when experiencing hemorrhage. It is normal for the patient to have mood swings. In such situations, the nurse ought to stay with the patient and inform the family of the patient to provide the best support to her during this period. The patient requires both physical and mental support.
Educate the patient about her condition:
It is crucial to listen and assess how much the patient knows about her health and how well she can take care of herself. The nurse will educate the mother about her breastfeeding techniques, her medications, the cause of the hemorrhage, how to deal with the pain at home, and what to do in case of an emergency. The mother should report to the hospital if she notices anything unusual.
Related: Best Postpartum Underwear-12 Most Comfortable & Maximum Absorbency Underwear
Source:






5 Replies to “Postpartum Hemorrhage Nursing Diagnosis-Risks-Care Plan-Management”